Essentials for Social Justice: Close the Gap
Archived
You are in an archived section of the website. This information may not be current.
This page was first created in December, 2012
Essentials for Social Justice: Close the Gap
Tom Calma
Aboriginal and Torres Strait
Islander Social Justice Commissioner and
Race Discrimination
Commissioner,
Human Rights and Equal Opportunity Commission.
11 June 2008
Collaborative Indigenous Policy Development
Conference, Brisbane.
Essentials for Social Justice
Between December 2007 and July 2008 the Aboriginal and Torres Strait Islander Social Justice Commissioner, Tom Calma, will deliver a series of key speeches setting out an agenda for change in Indigenous affairs.
Good morning.
Slide 1
Essentials for Social Justice:
Close the Gap
Tom Calma, Aboriginal and Torres Strait Islander Social Justice Commissioner, Human Rights and Equal Opportunity Commission
The Hon. Warren Snowden MP, distinguished guests and friends from across
Australia.
I begin by paying my respects to the Jagera and Turrubual peoples, the
traditional owners of the land where we gather today. I pay my respects to your
elders, to the ancestors and to those who have come before us. And thank you
Maruchi for your generous welcome to country for all of us.
This speech is the fourth in a series of six that I will be delivering
nationally outlining an agenda for change across all areas of Indigenous
affairs. I have termed this series of speeches Essentials for Social
Justice.
The first speech in this series was titled “Sorry” and outlined
an agenda for addressing the needs of the stolen generations and the delivery of
a national apology. The second – “Reform” - focused on the
need for structural reform within government so that government is capable of
meeting its commitments and ambitions. The third – “Protecting
Indigenous children” – focused on addressing family violence and
child abuse and the NT intervention.
Today’s speech is titled “Close the Gap” - a title that is
a lot more popular now than it was when I started using it a couple of years
ago.
Remaining speeches in the essentials for social justice series in the
coming months will address the importance of land and culture in creating
economic development; and a look back at the progress of the Rudd government
over its first 8 months in office.
But today - Close the Gap. So, what then is the gap being referred to?
why does it need closing? what does it have to do with “Collaborative
Indigenous Policy Development? and what lessons can the Close the Gap campaign
offer Indigenous affairs more generally?
The gap is the big one between the health status and life expectation of
Indigenous and non-Indigenous Australians.
Slide 2
'It is not credible to suggest that one of the wealthiest nations of the world cannot solve a health crisis affecting less than 3% of its citizens'
It is well known for example that there is an estimated difference of
approximately 17 years between Indigenous and non-Indigenous life expectation.
To look at this another way, that means that 75% of Indigenous males and 65% of
females will die before the age of 65 years compared to 26% of males and 16% of
females in the non-Indigenous population. For all age groups below 65 years,
the age-specific death rates for Indigenous peoples were at least twice those
experienced by the non-Indigenous population.
Slide 3
Health inequality – a snapshot
See: Australian Bureau of Statistics, Australian Institute of Health and Welfare: The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples (2005)
Life expectation:
There is an estimated 17 year gap between Indigenous and
non-Indigenous people (1996–2001).
Death age and rate:
For all age groups, Indigenous people are dying at twice
the rate of non-Indigenous people (1999-2003).
Infant and child health:
Twice the number of low birth weight babies are born to Indigenous women when compared to non-Indigenous women (2000-02); Indigenous infant mortality is up to 3 times the non-Indigenous rate (1999-2003).
In fact, there are a number of disturbing indicators and
trends that reveal an entrenched health crisis in the Indigenous population that
need addressing if this gap is to close:
- High rates of chronic diseases such as renal failure, cardio-vascular
diseases and diabetes. In 1999–2003, two of the three leading causes of
death for Indigenous people in Queensland, South Australia, Western Australia
and the Northern Territory were chronic diseases of the circulatory system and
cancer.
- High rates of poor health among Indigenous infants do not bode well
for the future adult population. In 2000-02, babies with an Indigenous mother
were twice as likely to be low birth weight babies (those weighing less
than 2,500 grams at birth) as babies with a non-Indigenous mother.
- High rates of unhealthy and risky behaviour, including an increased
prevalence of substance abuse and alcohol and tobacco use in the Indigenous
population.
With a significant proportion of Indigenous peoples in younger age
groups, there is an additional challenge to programs and services being able to
keep up with the future demands of a burgeoning population. Unless substantial
steps are taken now, there is a very real prospect that the health status of
Indigenous peoples could worsen and the gap get bigger still.
So that is the ‘gap’ I am referring to: a health status gap that
divides the life experience of black and white Australians. I will not be the
first to observe that the situation is something like having two nations in one:
on one hand the non-Indigenous population enjoying some of the best health in
the world, and - at the other end - the Indigenous population being forced to
settle for something far less.
And behind this gap, there are other divides. Most importantly a divide
between the opportunities to be healthy presented to black and white
Australians. And I think this is a vital point to realise - particularly for
those who would blame Indigenous peoples for their own poorer health. For while
it is true that we are all ultimately responsible for the choices we make that
affect our health, it is equally true that for a variety of reasons Indigenous
Australians have fewer choices to make for health than other Australians.
For example, given that Indigenous peoples’ poorer health status would
indicate a greater need for primary health care services, it is disturbing that
in 2004 it was estimated that Indigenous peoples enjoyed 40% of the per capita
access of the non-Indigenous population to primary health care provided by
mainstream general practitioners. In other words, many Indigenous peoples
cannot make the same kind of choices to see a doctor when they are ill, be
checked up, or take advice from doctors about healthy living. And there are
many reasons for this. Because a higher proportion of the Indigenous population
live in rural and remote areas, the doctor shortage in the bush is having a
greater impact on Indigenous peoples when compared to the non-Indigenous
population, for example.
But even in the urban centres, where the majority of Indigenous Australians
live, they choose against using mainstream primary health care even where it is
otherwise available and physically accessible. This can be for many reasons
including a lack of cultural ‘fit’, language barriers, or the
perception that mainstream services are not welcoming to Indigenous peoples.
Australian governments have long accepted the importance of maintaining distinct
health services in urban centres for Indigenous people as a consequence of this.
Per capita Medicare under spend estimates have been used to assess the
quantum of the Indigenous primary health care shortfall. Estimates of the
shortfall range from $250 million per annum to $570 million per annum depending
on the quality of service offered. So in an era of record ten and twenty
billion dollar budget surpluses, we are not talking big sums to close this
particular divide.
Another area where there is a divide is in relation to health infrastructure,
a term used here to describe all the things that support good health, but that
are not health services. Examples include: potable water supplies, healthy
food, healthy housing, sewerage and sanitation, and so on.
The dominant feature of health infrastructure inequality in Australia relates
to Indigenous peoples’ housing. Nationally, 5.5% of Indigenous households
live in overcrowded conditions. The proportion of overcrowded households was
highest for those renting from Indigenous or community organisations (25.7%).
Among the jurisdictions, the proportion of overcrowded households was highest in
the Northern Territory (23.7%)
In relation to health infrastructure, a century of neglect of health
infrastructure in Indigenous communities has left what could be a $3-4 billion
project for this generation, but again - in the scheme of things -- these sums
should not discourage us, particularly if one thinks of a ten year program, for
example, over which the overall cost would be spread.
And, of course, a wide range of social factors (such as income, education and
so on) also determine good or bad health in a population group. Research has
demonstrated associations between an individual’s social and economic
status and their health. In short, poverty is clearly associated with poor
health. And as is well known, Indigenous peoples in Australia experience
socio-economic disadvantage on all major indicators.
And there are other divides too. While poverty is an example of a social
determinant that will impact on both Indigenous and non-Indigenous Australians,
there are some social determinants evident in Australia that will only impact on
Indigenous peoples.
Slide 4
Our challenge for the future is to embrace a new partnership between Indigenous and non-Indigenous Australians. The core of this partnership for the future is closing the gap between Indigenous and non-Indigenous Australians on life expectancy, educational achievement and employment opportunities. This new partnership on closing the gap will set concrete targets for the future: within a decade to halve the widening gap in literacy, numeracy and employment outcomes and opportunities for Indigenous children, within a decade to halve the appalling gap in infant mortality rates between Indigenous and non-Indigenous children and, within a generation, to close the equally appalling 17-year life gap between Indigenous and non-Indigenous when it comes to overall life expectancy.
Prime Minister Kevin Rudd, Apology to Australia’s Indigenous Peoples, 13 February 2008
The unfinished business of colonisation and ongoing second
class status afforded Indigenous peoples in Australian society is an example.
This includes the stalled efforts to reconciliation (hopefully reignited by the
recently offered National Apology to the Stolen Generations), and the ongoing
uncertainty surrounding the issues of land, control of resources, cultural
security, the rights of self-determination and sovereignty.
Racism too is likely to affect the social and emotional (as well as mental
and physical) health of Indigenous Australians in a way not experienced by most
other Australians.
So the gap I am referring too, the gap in the health status and life
expectation enjoyed by non-Indigenous and Indigenous Australians, can be
conceived of as a manifestation of other divides that exist in areas like
health services provision, health infrastructure and broader social and economic
factors that narrow the choices for health that Indigenous Australians can make.
And all these must be addressed if the health status and life expectation gap
between black and white Australia is to close.
Slide 5
Social Justice Report 2005
Achieving Aboriginal and Torres Strait Islander health equality within a generation – A human rights based approach
In my 2005 Social Justice Report, I argued that it was
unacceptable for a country as rich as ours, and one based on the notion of the
‘fair go’ and the ‘level playing field’, to tolerate the
gap, or the divides that underlie it.
The 2005 report set forth a human rights based approach to achieving
Aboriginal and Torres Strait Islander health equality within a generation.
It made three recommendations to this end.
Slide 6
Recommendation One
Governments of Australia commit to achieving equality of health status and life expectation between Aboriginal and Torres Strait Islander and non-Indigenous people within 25 years.
The first recommendation was that the governments of
Australia commit to achieving equality of health status and life expectation
between Aboriginal and Torres Strait Islander and non-Indigenous people within
25 years.
Slide 7
Recommendation Two
Governments of Australia commit to achieving equality of access to primary health care and health infrastructure within 10 years for Aboriginal and Torres Strait Islander peoples
The second recommendation set out a process for what would
need to occur for this commitment to be met. It called for:
- The governments of Australia to commit to achieving equality of access to
primary health care and health infrastructure within 10 years for Aboriginal and
Torres Strait Islander peoples; - The establishment of benchmarks and targets for achieving equality of health
status and life expectation - negotiated with the full participation of
Aboriginal and Torres Strait Islander peoples, and committed to by all
Australian governments;
Slide 8
Recommendation Two cont.
- Establishment of benchmarks and targets negotiated with the full participation of Aboriginal and Torres Strait Islander peoples.
- Resources to be made available through mainstream and Indigenous specific services, so that funding matches need in communities and is adequate to achieve the benchmarks, targets and goals.
- A whole of government approach to be adopted to Indigenous health, including by building the goal and aims of the National Strategic Framework for Aboriginal and Torres Strait Islander Health into the operation of Indigenous Coordination Centres regionally across Australia
- Resources to be made available for Aboriginal and Torres Strait Islander
health, through mainstream and Indigenous specific services, so that funding
matches need in communities and is adequate to achieve the benchmarks, targets
and goals set out above; and - A whole of government approach to be adopted to Indigenous health, including
by building the goals and aims of the National Strategic Framework for
Aboriginal and Torres Strait Islander Health into the operation of Indigenous
Coordination Centres regionally across Australia.
The final recommendation then recommended that the Australian
Health Minister’s Conference agree to a National Commitment to achieve
Aboriginal and Torres Strait Islander Health Equality and that bi-partisan
support for this commitment be sought in federal Parliament and in all state and
territory parliaments.
That was two years ago.
Since the release of the Report I have been working with a growing coalition
of organisations who have committed to working in partnership to see these
recommendations implemented.
Slide 10
Campaign members
- NACCHO
- Australian Indigenous Doctor’s Association
- Australian Medical Association
- ANTaR
- Oxfam Australia
- CRC Aboriginal Health
- Australian General Practice Network
- Royal Australian College of General Practitioners
- Indigenous Dentists Association
- CATSIN
It encompasses every major Indigenous and non-Indigenous
peak health body in the country, as well as reconciliation groups, human rights
organisations and NGOs. It is an extraordinarily committed group of
organisations and individuals, across a vast array of different sectors of the
community.
The campaign progressed over the past 2 years without any financial support
from Australian governments - it has been self-funded.
Slide 11
Campaign members cont
- Heart Foundation of Australia
- Reconciliation Australia
- Royal Australasian College of Physicians
- Public Health Association of Australia
- Indigenous Nurses Association
- Rural Health Alliance
- Fred Hollows Foundation
- Ian Thorpe Foundation for Youth
- Telethon Institute
- Jimmy Little Foundation
- Many others
Overall, the campaign has been led by a leadership group
comprising the National Aboriginal Community Controlled Health Organisation, the
Australian Indigenous Doctors’ Association, the Congress of Aboriginal and
Torres Strait Islander Nurses, the Indigenous Dentists’ Association of
Australia, Oxfam Australia and HREOC.
‘Close the Gap’ was the public title for the Campaign.
One of our primary aims at the time was to obtain the commitment of all
Australian governments – through COAG – and of the Australian
government in particular due to its significant responsibilities for primary
health care - to commit to closing the gap on Indigenous life expectancy within
a generation. And it was to obtain this commitment on a basis of partnership
and shared ambition with a wide range of sectors of the community.
As you will be aware, the Councils of Australian Governments did exactly that
on 20 December 2007.
In their Communiqué they state:
Slide 12
Our window of opportunity
We currently have an opportunity to achieve lasting change in Indigenous health.
We will only seize this opportunity by working together.
COAG agreed the 17 year gap in life expectancy between Indigenous and
non-Indigenous Australians must be closed.COAG today agreed to a partnership between all levels of government to work
with Indigenous communities to achieve the target of closing the gap on
Indigenous disadvantage.COAG committed to:
- Closing the life expectancy gap within a generation;
- Halving the mortality gap for children under five within a decade; and
- Halving the gap in reading, writing and numeracy within a decade.
The first stage of the Close the Gap Campaign culminated in the
National Indigenous Health Equality Summit held in Canberra over 18 – 20
March, 2008. There were two streams of activity that took place at the Summit:
Slide 13
National Indigenous Health Equality Summit –
The challenge
- Government acceptance of primary health care and health infrastructure ten year targets:
- Realistic yet ambitious targets should be put in place for specific health issues;
- An ongoing partnership between governments and Indigenous health service peaks and other relevant bodies
- First, a series of Indigenous Health Equality Targets were extensively
workshopped to provide the means by which commitments to close the gap can be
met.
- Second, the Commonwealth government and the Opposition were invited to
formally re-commit to achieving Indigenous health equality within a generation.
Slide 14
National Health Equality Summit
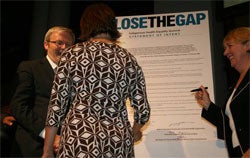
On 20 March 2008 the Summit concluded in the
Great Hall of Parliament House with a formal ceremony at which a Statement of
Intent was signed by the Prime Minister, the Ministers for Health and
Indigenous Affairs, the Opposition leader, and every major Indigenous and
non-Indigenous health peak body across Australia.
This Statement of Intent commits each of these bodies to a new partnership to
close the gap. It states:
Slide 15
Statement of Intent – 20 March 2008
We are:
- Representatives of the Australian Government
- National Aboriginal Community Controlled Health Organisation
- Congress of Aboriginal and Torres Strait Islander Nurses
- Australian Indigenous Doctors Association
- Indigenous Dentists Association of Australia
- Aboriginal and Torres Strait Islander Social Justice Commissioner
We share a determination to close the fundamental divide between the health
outcomes and life expectancy of the Aboriginal and Torres Strait Islander
peoples of Australia and non-Indigenous Australians.We are committed to ensuring that Aboriginal and Torres Strait Islander
peoples have equal life chances to all other Australians.We are committed to working towards ensuring Aboriginal and Torres Strait
Islander peoples have access to health services that are equal in standard to
those enjoyed by other Australians, and enjoy living conditions that support
their social, emotional and cultural well-being.We recognise that specific measures are needed to improve Aboriginal and
Torres Strait Islander peoples’ access to health services.Crucial to ensuring equal access to health services is ensuring that
Aboriginal and Torres Strait Islander peoples are actively involved in the
design, delivery, and control of these services.
Slide 16
Statement of Intent – 20 March 2008
Accordingly we commit:
- To developing a comprehensive, long-term plan of action, that is targeted to need, evidence-based and capable of addressing the existing inequities
- in health services, in order to achieve equality of health status and life expectancy between Aboriginal and Torres Strait Islander peoples and non- Indigenous Australians by 2030.
- To ensuring primary health care services and health infrastructure for Aboriginal and Torres Strait Islander peoples which are capable of bridging thegap in health standards by 2018.
Slide 17
- To ensuring the full participation of Aboriginal and Torres Strait Islander
peoples and their representative bodies in all aspects of addressing their
health needs.
- To working collectively to systematically address the social determinants
that impact on achieving health equality for Aboriginal and Torres Strait
Islander peoples.
- To building on the evidence base and supporting what works in Aboriginal and
Torres Strait Islander health, and relevant international experience.
Slide 18
- To supporting and developing Aboriginal and Torres Strait Islander
community-controlled health services in urban, rural and remote areas in order
to achieve lasting improvements in Aboriginal and Torres Strait Islander health
and wellbeing.
- To achieving improved access to, and outcomes from, mainstream services for
Aboriginal and Torres Strait Islander peoples.
- To respect and promote the rights of Aboriginal and Torres Strait Islander
peoples, including by ensuring that health services are available, appropriate,
accessible, affordable, and of good quality, and
- To measure, monitor, and report on our joint efforts, in accordance with
benchmarks and targets, to ensure that we are progressively realising our shared
ambitions.
This is a major development and one that we now need to work
together to capitalise on. Many people see this as a watershed in Indigenous
policy – so the time is now to realise our goals and seize this
moment.
To progress this new partnership, the Summit also finalised a series of
targets to close the health inequality gap. These targets note that the
achievement of the COAG goals requires a far more effective approach to
Aboriginal and Torres Strait Islander health and in particular, those factors
which are major contributors to current gaps in child mortality and the life
expectancy gap.
Slide 19
Close the Gap targets
These are grouped under four broad headings:
- Partnership Targets – to lock into place a collaborative approach to Indigenous health;
- Targets that focus on specific priority areas of child and maternal health, chronic disease and mental health and emotional and social wellbeing;
- Primary Health Care and other Health Services Targets and
- Infrastructure Targets.
We have therefore developed an integrated set of Close the
Gap targets. These targets are grouped under four broad headings:
- Partnership Targets - to lock into place a collaborative approach to
Indigenous health; - Targets that focus on specific priority areas of child and maternal health,
chronic disease and mental health and emotional and social wellbeing; - Primary Health Care and other Health Services Targets; and
- Infrastructure Targets.
And we emphasise that ‘cherry picking’ specific targets
or illnesses will not achieve the COAG goals.
Instead, we place far more reliance on integrated approaches to achieve the
goals of equal access for equal need and equal health outcomes.
We argue that it is of limited value to say a particular condition or factor
is important unless it is clear what the health target is, how it is to be
achieved, indicative expenditure required (both recurrent and capital), program,
workforce and infrastructure requirements to provide the necessary services and
the monitoring, evaluation and management processes required.
The integrated sets of targets are designed to deal with these requirements,
and mark a turning point for Aboriginal and Torres Strait Islander services. In
particular as agreed by COAG, a partnership approach is proposed, involving
Aboriginal people and their representative bodies, health agencies, government
agencies and the wider community.
These targets should be seen as the first step in a continuing process, where
their refinement and implementation can be conducted through a genuine
partnership between government and Aboriginal and Torres Strait Islander and
other organisations.
The details of the structure and processes of this partnership will have to
be determined and are essential to the achievement of the COAG goals. A fresh
Government approach to partnership and to its management, monitoring, evaluation
and review processes is essential for the achievement of the COAG goals - a
little bit more of the same will not close the gap.
These targets will be formally presented to the government and publicly
released in the coming weeks. We are currently working with COAG Working Groups
to ensure that the targets can be integrated into the COAG reform agenda for
Indigenous issues.
And so, I want to conclude by considering the essential components for
Closing the Gap in Indigenous health. But I would like to point out that these
essential components are relevant to all aspects of Indigenous affairs policy,
programs and service delivery.
Slide 20
Essential Components
- Partnerships
- Participation
- Prioritising
- Integrated and coordinated services
- Adequate resourcing
- Reforms to financing models and data collection methods
The first is a principle of broad application. That is, the need for
partnership. This is what the Statement of Intent for a new partnership
is all about.
We can’t achieve health equality by treating this as an issue solely
for government to address, or solely for Indigenous peoples.
I believe we have now reached a point where people have begun to be convinced
that achieving health equality is achievable. This is what the evidence tells
us, even if we lost faith over the past decade.
So such partnership requires an honesty and integrity about what needs to
occur and transparency about how we are travelling, and whether we are doing
everything we can to achieve our longer term goal.
Secondly, we need to ensure the full participation of Indigenous peoples in
policy making processes and health programs in particular. We need to adopt a
proactive approach to Indigenous health that has a prevention focus and builds a
comprehensive primary health care approach.
Third, and related to this, is that high quality, integrated primary health
care should be prioritised.
A focus on primary health care interventions addressing chronic diseases can
be expected to have a significant impact on Aboriginal and Torres Strait
Islander peoples’ life expectation. Critically for the Indigenous
population, primary health care identifies and treats chronic diseases
(including diabetes, cardiovascular and renal disease) and their risk factors.
Primary health care also acts as a pathway to specialist and tertiary care, and
enables local (or regional) identification and response to health hazards;
transfer of knowledge and skills for healthy living; and identification and
advocacy for the health needs of the community.
There should also be continued support for Aboriginal community controlled
health services. There is evidence that they are a highly effective process for
the provision of primary health care. There should also be independent research
conducted to determine the success factors and governance issues which
contribute to achieving the most effective community controlled health services
possible.
The expansion of community controlled health services must take place
alongside efforts to improve the accessibility of mainstream services. It should
also be accompanied by health care programs focusing on specific diseases. If,
through these, early stage symptoms are detected not only can suffering be
prevented, but cost savings made.
The fourth requirement is that we integrate targets for health equality into
policy and programs across all governments. The Prime Minister announced at the
National Indigenous Health Equality Summit in March that a new National
Indigenous Health Equality Council will be established and operate from July
this year. Its role should include advising on the implementation of targets
and benchmarks. This provides an opportunity to embed the targets into policy
and practice nationally.
And this is very much a work in progress. The Steering Committee for the
Close the Gap Campaign continues to work with COAG and Australian governments to
progress the adoption of the targets, and their integration into the National
Strategic Framework for Aboriginal and Torres Strait Islander Health, the
Aboriginal and Torres Strait Islander Health Performance Framework and the
Productivity Commission’s Overcoming Indigenous Disadvantage framework.
It is hoped that in the near future these policy frameworks and indicators will
be linked to benchmarks and targets to achieve Indigenous health equality by
2030 or earlier.
There is sufficient evidence to demonstrate that a targeted approach will
work and that the improvements sought in Aboriginal and Torres Strait Islander
peoples’ health status are achievable. For example, a recent review of
Aboriginal primary health care states that:
international figures demonstrate that optimally and consistently resourced
primary health care systems can make a significant difference to the health
status of populations, as measured by life expectancy, within a decade. For
example, in the 1940s to the 1950s in the United States, Native American life
expectancy improved by about 9 years; an increase in life expectancy of about
twelve years took place in Aotearoa/ New Zealand over two decades from the 1940s
to the 1960s.
Figures from within Australia demonstrate dramatic improvements in infant
mortality (for example from 200 per 1,000 in the mid 1960s in Central Australia
to around 50 per 1,000 by 1980) through the provision of medical
services.1
The fifth essential is the adequate resourcing of commitments to Indigenous
health. Research suggests that addressing Aboriginal and Torres Strait Islander
health inequality will involve no more than a 1% per annum increase in total
health expenditure in Australia over the next ten years. If this funding is
committed, then the expenditure required is then likely to decline thereafter.
Only with funding commitments that are proportionate to the outstanding need
in communities will it be feasible for governments to meet the outstanding
primary health care and infrastructure needs of Aboriginal and Torres Strait
Islander communities within 10 years.
This has been acknowledged in the Statement of Intent which talks of funding
matching need to achieve equality.
Generally, primary health care is a responsibility of the federal government
- but savings made here can prevent engagement of Aboriginal and Torres Strait
Islander peoples with the secondary and tertiary systems, which are
predominately responsibilities of the states and territories. The states and
territories also have significant responsibilities for service delivery in areas
which impact on health outcomes, such as housing.
In light of the comprehensive national frameworks and strategies in place, it
would appear that there exists a solid basis for governments to work together to
address the projected funding shortfall. Additional funding to the states and
territories could be made contingent on the agreement of states and territories
to match federal contributions.
An equitable distribution of primary health care rests on a prior effort to
increase the numbers of health professionals, and particularly Indigenous health
professionals, to provide the services.
Any substantive address must begin at school – students must not only
complete school, but they must receive a thorough grounding in maths and science
to enter medicine. Recruitment campaigns must start focusing on Aboriginal and
Torres Strait Islander young people at an early age.
Finally, to support these commitments and proposed targets, further reform of
health financing models and data collection methods is required.
There has been significant work done to improve health financing models
towards processes that identify the level of need. For example, quantifying the
Medicare Benefit Scheme spending shortfall on Aboriginal and Torres Strait
Islander peoples has provided a basis for quantifying the primary health care
shortfall and stimulated initiatives to ensure Aboriginal and Torres Strait
Islanders enjoy greater access to Medicare and the Pharmaceutical Benefits
Scheme. Further work is required to quantify and enable the level of need to be
quantified nationally, as well as at a regional and sub-regional level for both
primary health care access and health infrastructure provision.
Ultimately, there is no larger challenge to the sense of decency, fairness
and egalitarianism that characterizes the Australian spirit, than the current
status of Aboriginal and Torres Strait Islander health. Closing the Gap is not
only a major human rights issue in Australia, but it should be a matter of pride
for us all.
And Closing the Gap is not impossible, although it will require long term
action and commitment.
Committing to a year 2030 time frame to achieve this is feasible. It is also
a long time in which to accept that inequality would continue to exist.
But history shows us that an absence of targeted action and a contentedness
that we are ‘slowly getting there’ is not going to result in the
significant improvements in health status that Aboriginal and Torres Strait
Islander peoples deserve - simply by virtue of the fact that we are members of
the human race and of the Australian community.
We have an unprecedented opportunity to make this happen due to the recent
commitments of Australian governments and the adoption of national Indigenous
Health Equality targets, but targets on their own will not suffice - we need
action on many fronts to address the many divides that lay behind the gap. And
we do need to augment current efforts.
The failure of the policies and programs of the past twenty years to achieve
significant improvements in Aboriginal and Torres Strait Islander health status,
yet alone to close the gap, reveal two things that Aboriginal and Torres Strait
Islander peoples and the general community can no longer accept from
governments.
First, we can no longer accept the making of commitments to address
Aboriginal and Torres Strait Islander health inequality without putting
into place processes and programs to match the stated commitments. Programs and
service delivery must be adequately resourced and supported so that they are
capable of achieving the stated goals of governments.
Second, and conversely, we can also not accept the failure of governments to
resource programs properly. A plan that is not adequately funded to meet its
outcomes cannot be considered an effective plan. The history of approaches
to Aboriginal and Torres Strait Islander health reflects this.
The combination of the healthy economic situation (at least in terms of the
surpluses) of the country, the substantial potential that currently exists in
the health sector and the national leadership being shown through the COAG
process, means that the current policy environment is ripe for achieving the
longstanding goal of overcoming Aboriginal and Torres Strait Islander health
inequality. Steps taken now could be determinative.
The gap - the Indigenous health equality gap - can be closed, and closed in
our lifetimes. The foundations are in place, but none of us can afford to rest
on our laurels - it is imperative that we hold Australian governments to their
commitments so that by 2030 any Indigenous child born in this country has the
same chances as his or her non-Indigenous brothers and sisters to live a long,
healthy and happy life.
Slide 21
Essentials for Social Justice speeches
Please visit the HREOC website to download the other speeches in the Essentials series
- 11 December 2007: Sorry
- 20 February 2008 : Reform
- 31 March 2008: Protecting Indigenous children
http://www.humanrights.gov.au/social_justice/essentials/index.html
Thank you.
Note: This is the fourth in a series of six speeches outlining an
agenda for change in Indigenous Affairs. The “Essentials for Social
Justice” series will be presented between December 2007 and July 2008,
and will be available online at: www.humanrights.gov.au/social_justice/essentials/index.html
[1] Dwyer, J., Silburn, K. and
Wilson, G., op.cit., p40.
